You’ve been told that you have throat cancer and need a total laryngectomy. Here are 11 things you need to know before getting the operation.
Short back story: I was diagnosed with throat cancer in March of 2022. I had a total laryngectomy in early April of that year.
From the time of my diagnosis and second opinion, to me being on an operation table getting my neck sliced open and voice box, part of my thyroid, and some lymph nodes removed, I had just a few days to learn all I could about what was going to happen to me.
Needless to say, I know a whole lot more since I became a “Lary” than I did before the surgery.
Some people have more time, some less. Recently someone told me how they were taken to a hospital in an ambulance and woke up a Lary.
So, with that, let’s run down what you need to know before you have the laryngectomy.
Note: some of these come from my experience, and some from other laryngectomees.
What Is A Laryngectomy?
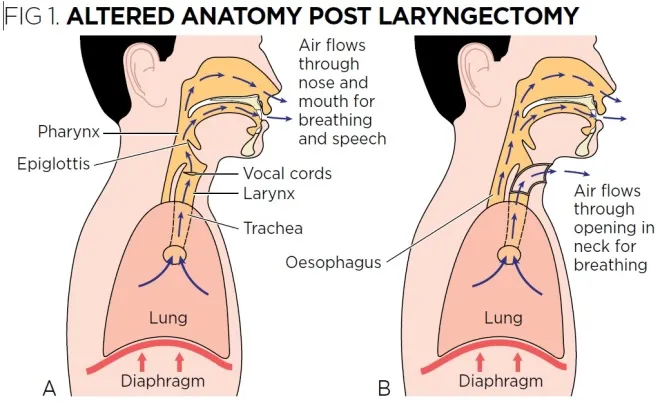
A total laryngectomy (“TL”) is the removal of one’s vocal chords and reconstruction of the trachea (windpipe) and esophagus (food pipe).
A partial laryngectomy, which is less common, is the removal of part of the vocal cords, leaving the trachea and esophagus intact. This procedure is less common than a total laryngectomy, so for this article I’m going to focus on the TL.
How Is The Throat Reconstructed?
The trachea and esophagus are reconstructed using tissue taken from somewhere else on the body (called the “donor site”). In my case it was the left forearm, but the shoulder, thigh, and chest areas are sometimes used. Then, a portion of the top layer of skin (the epidermis) from somewhere like the upper thigh, is used to graph over the donor site so it can begin to heal.


What’s left is a complete separation of the trachea and esophagus, with the esophagus going up to the head as usual, and the trachea coming out of a hole in the neck area. That hole is called a “stoma.”
Your surgeon should tell you what they plan on having to remove. If not, ask them. Mine did, but also said he wouldn’t know completely until he got in there.
Speech After A Laryngectomy
Unable To Speak
After a total laryngectomy, the patient is unable to talk. This is because a) there are no vocal chords, and b) even if there were, no air passes through the throat since you will breathe through your stoma.
Electrolarynx
There are ways to help us speak. One is an Electrolarynx (“EL”), which is a device that is pressed to the neck. It emits a buzz which the Lary can form into words. I have some difficulty using an EL, since I still have some fibrosis from lymphedema that prevents getting a good connection to my throat. (More about lymphedema below).
There are some that have mastered the EL. See this video from Tony Talmich.
Esophageal Speech
Another way of talking is Esophageal Speech (“ES”). In that method, the person injects a bit of air into the esophagus and then forces it out. It vibrates the tissue in the throat. Kinda like when we were kids, we would talk when we burped. This is a bit difficult to learn. I haven’t been able to master it yet.
TEP
A TEP, which stands for TransEsophageal Puncture, is where a surgeon pokes a hole in the trachea and into the esophagus. Then a small one-way valve (also called a TEP) is inserted into the hole. This allows the person to force air through the valve which, like ES, vibrates tissue in the throat. The one-way valve allows air to flow one way, into the esophagus, but prevents liquids from flowing from the esophagus into the windpipe.


I had my TEP procedure this past April, a year after my surgery. This is the way I speak now. It has some limits, which I will detail in a later article.
Boogie Board
A boogie board is a small tablet that you can write on and erase. You will need this, a plain old pencil and paper, or a phone app as you won’t be able to use any of the other means above in the beginning.

Atos gave me one, and you can also get one from Amazon here.
Phone App
There are quite a few text to speech phone apps. I installed this one before my surgery. Funny, but most of the doctors and nurses in the hospital had never seen anyone use one.

You can get it on Android here, and Apple here.
Record your voice
One tip people give is to record your voice before your operation. I didn’t, and wish I had.
Authorization To Speak
Also, since you won’t be able to talk on the phone, someone needs to be able to talk for you. Get with your doctors, the hospital, your insurance provider, etc. to give your caregiver authorization to speak on your behalf.
Unable To Smell
A Lary cannot smell, or can barely smell. This is not because there is a problem with the olfactory system, but rather, since no air passes through the nose, the smells cannot be detected.
Sometimes when cooking, the steam from the dish lets me smell a bit, or when the wind or a fan blows something my way I get a whiff. The other day I was cutting the grass on my riding lawn mower when it began to sprinkle. The breeze blew some air my way and I smelled wet grass. I have to admit I cried a little at being able to smell something that most people take for granted.
There is also a way we learn to smell some. It’s called the “polite yawn.” Basically we close our mouth and lower our bottom jaw like we were yawning. This sucks in a small amount of air through our nose, which enables us to detect some smells.
Here’s another way to smell from Bill Cross. He is speaking using a TEP.
Diminished Taste
With the sense of smell pretty much eliminated, this causes a diminished sense of taste. I’ll get into the taste thing later in the article.
What Kind Of Supplies Will I Need?
Ah, supplies. One of the hurdles we face. What will you need? Where do you get them? And what do they cost?
What Supplies Do I Need
This can vary from patient to patient. All depending on how far out they are from their surgery, and what if any issues they are having.
In a future article I’ll go over these supplies. what they are and what they do.
In the beginning you will need:
- Lary Tubes (this goes in the stoma to help keep it open)
- Collars (to hold the tube)
- HMEs (these small disks replicate the function of the nasal cavity in warming and moisturizing the air you breathe. They go in a Lary tube, button, or baseplate)
- Lubricant (to make it easier to insert the Lary Tube. Good old KY Jelly works great)
- Saline bullets (to help keep the airway clear)
- Brushes (to clean the tube)
- Aquaphor / Silvadene (for radiation burns if you go through radiation treatment)
- Later you may graduate to:
- Lary Clips (small adhesive pads with hooks on them to hold the tube)
- Lary Button (Like a Lary Tube but smaller and less intrusive)
- Baseplates ( to hold the HME when you no longer need a tube or button)
- Adhesive Remover (to help remove the baseplate without doing too much harm to the skin)
- Skin Protector (to help protect the skin from the baseplate adhesive)
- Tac Wipes or Glue (to help hold the baseplate on)
Some might need a suction machine. Maybe one for home and a portable one for on the go. And if you are in a very dry climate, a humidifier, as dry air isn’t good for the lungs.
Where do I Get Laryngectomy Supplies?
There are two main companies that provide laryngectomy supplies: Atos and InHealth. Some hospitals give you a sample pack from one of these companies. My hospital, Emory, gave me a case and a travel pack from Atos, but I’ve heard of other people, especially in smaller facilities, that don’t get much of anything. Some people have reported that they didn’t know much about what supplies they need, or where to get them.
In my opinion, that is a poor excuse for a hospital. One of their patients has just had a life altering procedure and they wind up leaving with nothing, not even knowledge.
It’s a good thing that we have organizations like Lary’s Speakeasy that provides needed supplies 100% free of charge, as well as education and information.
Who Pays For The Supplies?
Both Atos and InHealth accept medicare and most insurance plans, but sometimes they are not an in-network supplier. It was like that for me with Atos at first, but a few months later they became in-network. This cut what I was having to pay in half.
Both companies have patient advocates that can go to bat for you, and work with your insurance company.
Also both companies should be covered by medicaid, but that is on a state by state basis.
If you have a problem with supplies, join the Lary’s Speakeasy Facebook group and post a message. Someone there can usually help you. They have been a life saver for me. Not just for information, but to be able to connect with other Larys.
Radiation Treatment
Most people will go through radiation treatment (“RT”) after surgery. RT causes a lot of changes to your body. My oncologist explained a lot to me before I started, but I know a lot of people who didn’t get much information.
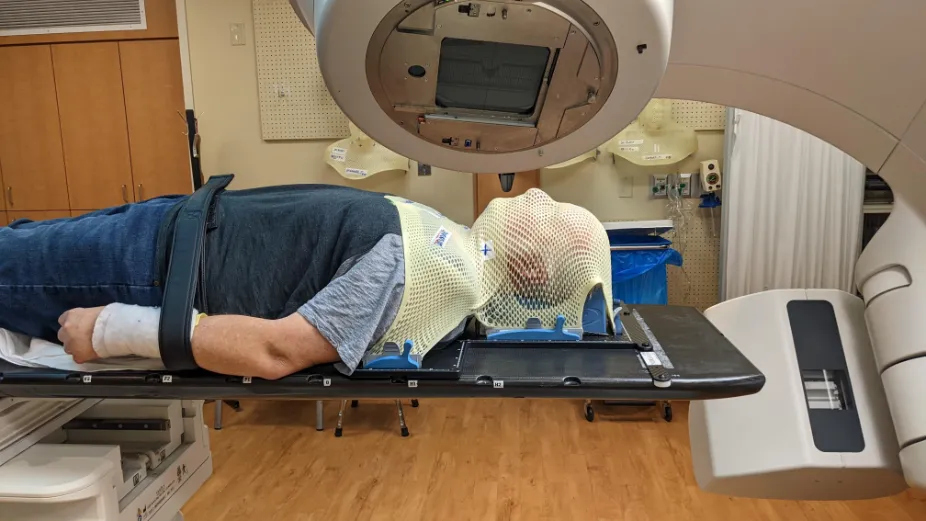
Duration Of Treatment
RT is usually 30 treatments that take just 5-10 minutes each. You will do this every day for six weeks. For me it was an hour drive to the hospital for a treatment that took at the most 20-30 minutes, if I had to wait a bit. Sometimes I was in and out in less than 15 minutes. Then an hour drive home.
Physical Effects
For the first 3 weeks you probably won’t notice any issues and will think this will be a walk in the park.
Then BAM! Things can start happening fast. You may experience:
Burns
Mild to extreme burns around your neck area. Use aquaphor on these and also Silvadene, but make sure nothing is on your neck area when you go in for a treatment. It can act like cooking oil and fry the skin.
HairLoss
Your hair could fall out. The hair on my head got pretty thin, and my beard fell out and still hasn’t grown back. It will grow as far down as my mouth, and from there down it’s pretty bare. The back of my neck is still as smooth as a baby’s butt.
Saliva
Your saliva could get thick and gummy, making your mouth feel dry. Some people said Xylitol liquid and lozenges help, but they didn’t work for me.
Loss of taste
I started losing my taste about three weeks into RT. From the time it started until total loss was less than a week. I couldn’t taste anything. I was drinking Pedialyte for hydration, but couldn’t tell you what flavor it was.
Combining the loss of taste with the thick saliva meant that anything I put in my mouth was like eating library paste. I tried different nutritional drinks to keep my calorie count up (my oncologist said I should take in around 2,000 calories a day) and finally found that Boost makes a high calorie drink. I lived on those for about 6 weeks.
But since my SLP (Speech-Language Pathologist) said I need to eat something solid every day, I had some pudding or fruit. Pudding or fruit that tasted like library paste.
Then one Sunday morning I woke up and took a sip of the Pedialyte I had sitting by the bed, and lo and behold I tasted lemon! I couldn’t taste it much, but I could taste it. From then on my taste started coming back and the saliva started getting thinner. Now 15 months out of RT I can say my taste is 90% of what it was.
Fatigue
Some people say they experience fatigue from radiation, but I didn’t. That came from chemotherapy (more about that below).
Thick Mucus
We all have mucus that collects on our Lary tube (and later button or baseplate), but radiation causes it to be especially thick and heavy. This is where the saline bullets come in.
Saline bullets are small plastic vials that contain a small amount of saline. They are designed to be able to squirt it into your stoma. This causes you to cough violently, but it helps to break up the mucus.
Some people also use a suction machine to help clear the airway.
These side effects of RT don’t stop when the treatment ends, they continue for a few weeks, maybe a year or more. Like I said, I’m over a year out and barely have to shave.
Chemotherapy
Not everyone goes through chemo, and some are more affected by it than others. I had 6 treatments (once a week) alongside my RT, and my issues were pretty mild compared to others.

Nausea
The biggest issue with chemo is nausea. They give you meds to help it, and I also received a prescription for a couple of different nausea medications. I only experienced nausea about three times, and that was while riding in the car. I popped a pill and about 20 minutes later it was gone.
Other people have different experiences, such as violently throwing up afterwards.
Tinnitus
Many people experience ringing in the ears because of the chemo. I did, and they changed to a different chemo drug which stopped it. I was told that if I had continued with the other drug it could cause permanent tinnitus and/or hearing loss.
Fatigue
Fatigue is another side effect of chemo. Some people have it more than others. For me, it started about halfway through the third day. I always had my treatments on a Monday, and by Wednesday afternoon I felt worn out. I was like that the rest of that day and all day Thursday. I couldn’t get out of bed. By Friday I was back to normal, only to do it again next week.
Lymphedema
Lymphedema is a big side effect of a Laryngectomy, for a couple of reasons.
Removal Of Lymph Nodes
I had a number of lymph nodes removed. I would have to go back to see how many. This can contribute to major lymphedema in the head and neck, as the body has to redirect fluid to other lymph nodes in the body.
Scar Tissue
The scar that runs from ear to ear also can block fluid from draining properly.
Therapy
I did, and you may, need to go to a lymphedema therapist. They can teach you how to help redirect the fluid.
Also, you may need to wear a compression mask at night, and maybe use a Flexitouch compression garment every day to help with the drainage. This is what I do, as well.

Physical Therapy
Why would someone need PT after a laryngectomy? Well, the surgery can do major damage to the shoulder area. I could barely raise my left arm afterward. PT helped me loosen it up, and getting back to the gym, which I did this past January, also helped. I can’t say that it’s 100%, but it’s close.
Also, my hand and wrist were weak from the forearm being the donor site. I had to work to strengthen them, as well.
So be prepared for some sessions with a physical terrorist therapist.
Dental Issues
One big effect of RT is the inability of the body being able to heal properly. You need a good assessment of any dental issues before undergoing a laryngectomy.
After RT, it is never advised to have any teeth pulled, as the bones in the jaw simply will not heal. So it’s best to have anything like that done before the surgery.
If your hospital cancer center has a dentist, I recommend using them. They will know a lot more than your family dentist.
Plus, you will be using high fluoride prescription toothpaste, and maybe a fluoride rinse as well, for the rest of your life.
Recurrence Of The Cancer
Some people go through all this, and the surgeon isn’t able to get all the cancer. It can only take a few cells for it to start spreading again.
A good surgeon will tell you this, but they won’t (or can’t) tell you what the probability of recurrence is.
This is why we have CT scans every 6 months. Best to try and catch something before it is able to spread. This can lead to “scanxiety” (yes, that’s a real thing). The worrying that sometimes comes right before a scan. What if they find something?
One of our contributors, Andrea No, wrote an article about that recently. You can find it here.
Depression
Depression is a biggie. This is a sudden life change for us. One day you can talk, the next day you can’t. Your main form of communication has been taken from you.
You later find ways to artificially speak, but it’s not really the same.
The rest of your life
The rest of your life will be different than it was. You can feel cut off from friends and family. Unable to join in on conversations like you used to. You can’t cheer for your grandkid’s baseball, football, basketball, or soccer team. It’s hard, if not impossible, to order at a drive thru. Talking on the phone is really only possible with a TEP, and then it’s difficult to be understood clearly.
An old friend of mine called me today and I was leary of answering the call, so I let it go to voicemail. I’ll text him later.
Physical Healing
We go through life with different ailments. We get colds or the flu. We have stomach viruses and sinus infections. Maybe we sprain ankles or break bones.
But we know that we’ll heal.
This is something that won’t heal. Our voice box ain’t growing back. The hole in our neck is permanent.
Sometimes We Feel Normal, Then We Don’t
Still, 18 months from my laryngectomy I sometimes forget that I can’t naturally talk. My wife will say something and I’ll try to answer her, and nothing comes out. Then I remember that I have to push the button on my HME to be able to say something. This can be a little depressing at times. Knowing that this is something I’ll have to deal with for the rest of my life.
It only lasts a fleeting moment, though. But for some it can be debilitating. I read what others sometimes write in the FB group, and I can feel the anger and/or depression in their voice. Don’t let this happen to you. You’re doing this for a reason. The reason is to stay alive. Alive, so you can go silently cheer for your grandkids.
Larry is the website and social media manager for Lary’s Speakeasy.
He also operates two blogs, Larry In Atlanta, which is mainly personal observations, and The Tech Boomer, which offers tech advice to seniors.
Larry and his wife, Denise live in the southern Metro Atlanta area. He had his laryngectomy in April, 2022.

Thanks, Larry. You hit the nail right on the head
Great work!
Thanks for the information Larry, I will be getting mine on Friday, I was aware of most of what you explained, so I’m grateful my ENT Dr has been thorough. I hope I can be helpful, as you are, a year after my laryngectomy. Stay sunny!!!
Thanks Larry you are a blessing and a inspiration 🙏👍😊
I cannot ad to this it’s absolutely perfect. Thank you from a 2 year Lary.
Nothing is said about a fistula, I didn’t know what it was until I had one. Not good.
Inspiring I had my TL 2nd of January this year. Most days are good, then I will look at old pics and see myself as I was and get a little melancholy, it soon passes and I’m back to my new self.
I never knew what a lary was, until the surgeon explained the morning of my
op. No choice to not go through with it, it was the op or death. Thanks for explaining it so eloquently much better than my surgeon ever did.